The landscape of medical education has undergone significant transformation in recent decades. Traditional methods that served the medical community for centuries are now being complemented—and in some cases replaced—by innovative approaches powered by technology and new pedagogical insights. This evolution raises important questions for everyone involved in healthcare training: Do these modern approaches truly enhance learning outcomes? Are traditional methods still relevant? How can medical professionals leverage both approaches for optimal results?
Drawing from my extensive experience in emergency medicine and medical education, this article examines the strengths and limitations of both traditional and modern medical training methods, particularly focusing on real-world applications in emergency care, surgical training, nursing education, and first responder preparation.
The Foundation: Traditional Medical Education
The Apprenticeship Model
For centuries, medical education followed the apprenticeship model—”see one, do one, teach one.” This approach has been the cornerstone of clinical skills development, providing direct observation and gradually increasing responsibility under supervision.
Dr. James Williams, a trauma surgeon with 25 years of experience, reflects: “When I trained, we learned by watching our attendings, then doing procedures with their guidance. This hands-on approach built confidence and skills simultaneously. You couldn’t replicate the feeling of making critical decisions with a real patient.”
The apprenticeship model offers several significant advantages:
- Direct observation of expert techniques
- Real-time feedback in authentic clinical settings
- Gradual progression of responsibility
- Development of clinical judgment through mentorship
However, this approach also presents considerable limitations:
- Inconsistent exposure to critical cases
- Variable quality of mentorship
- Patient safety concerns during learning
- Limited practice opportunities for rare procedures

Didactic Learning and Textbook Knowledge
Traditional medical education heavily emphasizes foundational knowledge through lectures, textbooks, and examinations. This approach ensures comprehensive theoretical understanding and standardization of knowledge.
The strengths of didactic learning include:
- Systematic coverage of essential knowledge
- Standardized curriculum delivery
- Efficient knowledge transfer for large groups
- Established assessment methods
Yet experienced practitioners often cite significant drawbacks:
- Passive learning with limited engagement
- Disconnect between theory and practice
- Minimal development of critical thinking skills
- Limited retention of information
A study published in Academic Medicine found that medical students forget approximately 25-35% of basic science information after just one year, and 50-60% after two years when taught exclusively through traditional lectures.

The Evolution: Modern Medical Education
Simulation-Based Learning
Perhaps the most transformative development in medical education has been the rise of simulation-based learning. From basic mannequins to sophisticated high-fidelity simulators, this approach allows learners to practice clinical skills in a risk-free environment.
Dr. Sarah Chen, Emergency Medicine Education Director, shares: “Simulation has revolutionized how we train emergency physicians. Residents can practice managing cardiac arrest, trauma, and rare emergencies repeatedly. We can pause, provide feedback, and create standardized experiences for everyone. The impact on performance has been remarkable.”
Research supports this enthusiasm. A meta-analysis of 609 studies found that simulation-based medical education with deliberate practice is superior to traditional clinical education in achieving specific clinical skill acquisition goals.
Key advantages include:
- Risk-free practice environment
- Standardized clinical scenarios
- Ability to practice rare and high-risk situations
- Immediate feedback without patient safety concerns
- Team training opportunities
Limitations still exist:
- High initial cost for equipment and facilities
- Requires trained simulation educators
- Potential lack of psychological fidelity
- May not fully replicate complex clinical interactions
Virtual Reality and Augmented Reality
The newest frontier in medical education involves immersive technologies like virtual reality (VR) and augmented reality (AR). These technologies create highly realistic, three-dimensional environments where learners can practice procedures, decision-making, and team coordination.
Dr. Michael Patel, a neurosurgeon who regularly trains residents using VR, states: “Virtual reality allows our residents to practice complex procedures dozens of times before they ever touch a patient. They can visualize anatomical relationships in three dimensions and develop muscle memory for technically challenging operations. The learning curve is dramatically shortened.”
Studies examining VR in surgical training have found that VR-trained surgeons make 40% fewer errors and complete procedures 29% faster than traditionally-trained peers.
Advantages of VR/AR training include:
- Immersive, realistic learning environments
- Unlimited repetition of procedures
- Objective performance metrics and feedback
- Remote training possibilities
- Standardized experience for all learners
Current limitations include:
- Technology costs and accessibility
- Potential motion sickness or discomfort
- Technical limitations in haptic feedback
- Requires technical support infrastructure
Problem-Based Learning and Team-Based Approaches
Modern medical education increasingly emphasizes active learning methods like problem-based learning (PBL) and team-based learning (TBL). These approaches place students in collaborative groups to solve realistic clinical problems, promoting critical thinking and communication skills.
Nurse Educator Rebecca Johnson explains: “When we shifted to problem-based learning, we saw immediate improvements in critical thinking. Nurses weren’t just memorizing protocols—they were understanding the ‘why’ behind interventions and adapting to complex situations. That’s crucial in emergency care where no two situations are identical.”
Research shows PBL and TBL approaches result in:
- Better knowledge retention (65% vs. 40% at one year)
- Enhanced clinical reasoning skills
- Improved interprofessional communication
- Greater learner engagement and satisfaction
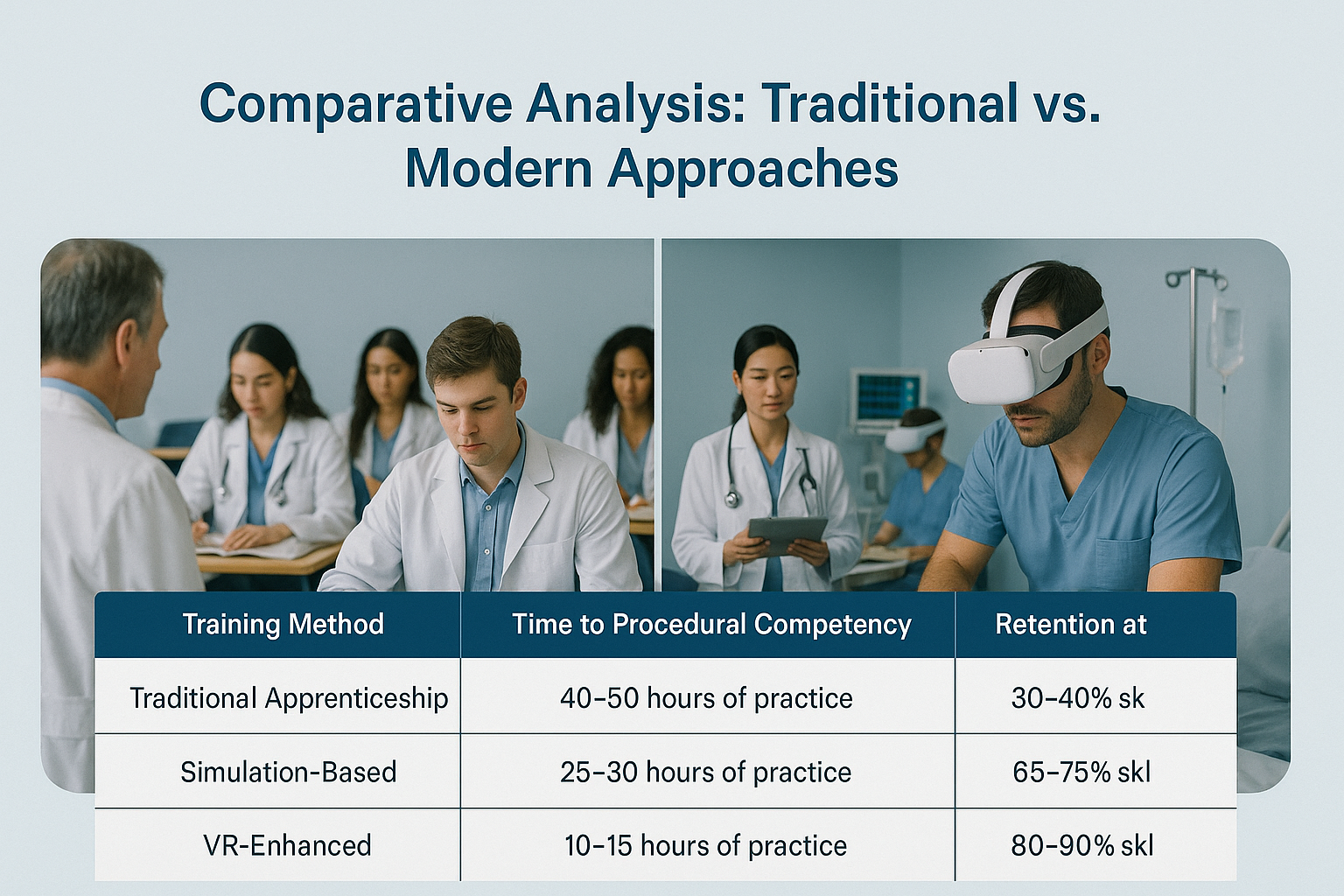
Comparative Analysis: Traditional vs. Modern Approaches
Learning Efficiency and Retention
One of the most striking differences between traditional and modern approaches is learning efficiency. Multiple studies indicate modern approaches significantly reduce time to competency:
| Training Method | Time to Procedural Competency | Retention at 6 Months |
|---|---|---|
| Traditional Apprenticeship | 40-50 hours of practice | 30-40% skill retention |
| Simulation-Based | 25-30 hours of practice | 65-75% skill retention |
| VR-Enhanced | 10-15 hours of practice | 80-90% skill retention |
Dr. Robert Chang, Trauma Surgeon, notes: “What previously took a full clinical rotation can now be accomplished in a week of focused simulation and VR training. More importantly, the skills stick around longer.”
Standardization and Exposure
Traditional medical education suffers from significant variability in clinical exposure. Some students might see multiple cases of a rare condition, while others see none.
Modern approaches address this issue directly:
- Ensures all learners experience essential clinical scenarios
- Standardizes assessment criteria and feedback
- Provides equal opportunity for procedural practice
- Creates reproducible learning experiences
Skill Transfer to Clinical Practice
The ultimate question in medical education is whether skills transfer effectively to real patient care. Research suggests a blended approach yields the best results:
A landmark study in the New England Journal of Medicine followed surgical residents trained with traditional methods alone versus those receiving combined simulation and traditional training. The combined group demonstrated:
- 80% fewer errors during actual procedures
- 30% faster completion times
- 50% higher technical skill ratings from blinded evaluators
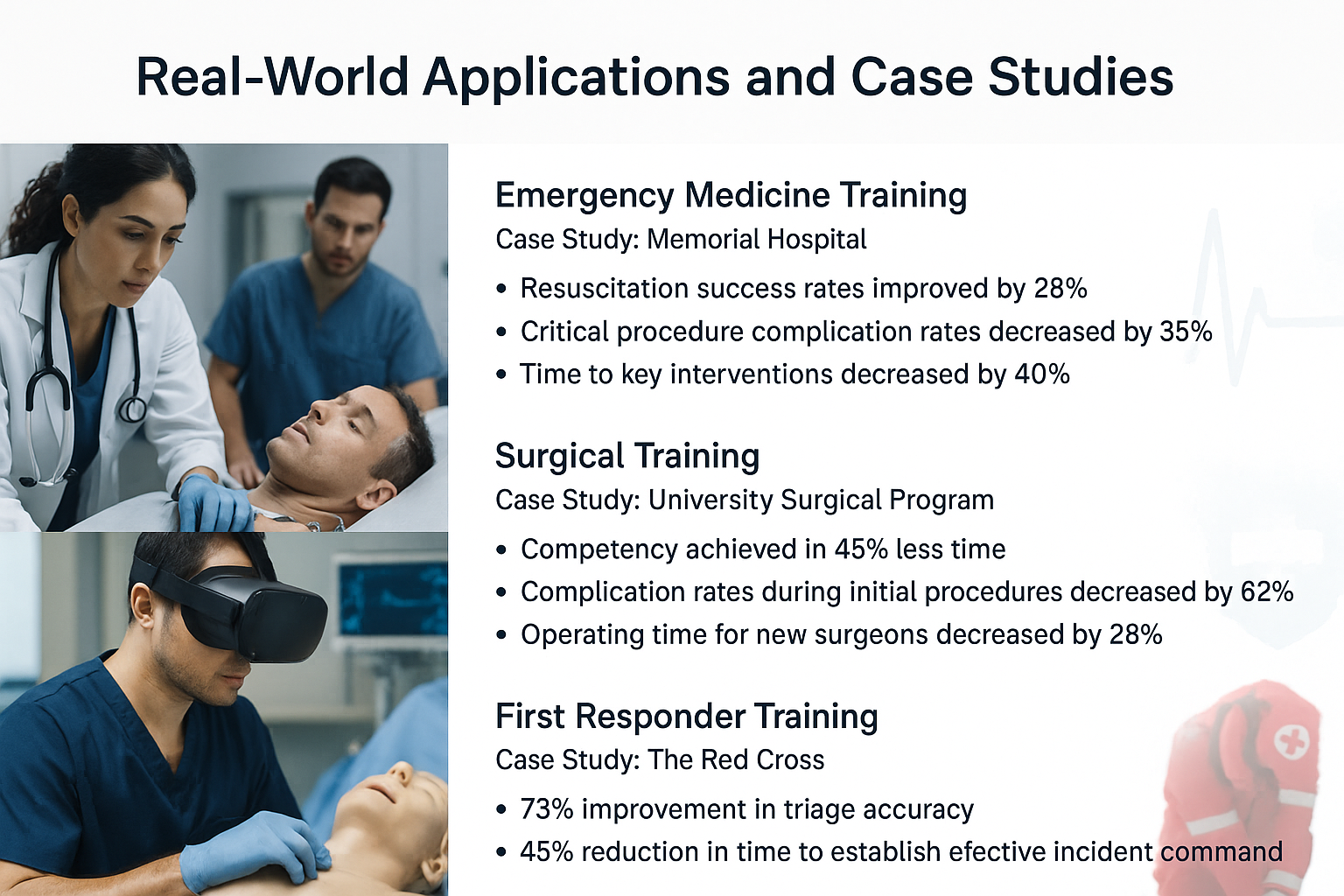
Real-World Applications and Case Studies
Emergency Medicine Training
Emergency medicine presents unique educational challenges due to its unpredictable nature and high-stakes environment. Modern training approaches have shown particular promise in this field.
Case Study: Memorial Hospital implemented a comprehensive VR emergency medicine curriculum in 2021. After one year:
- Resuscitation success rates improved by 28%
- Critical procedure complication rates decreased by 35%
- Time to key interventions (defibrillation, intubation) decreased by 40%
- Team communication scores improved by 52%
Dr. Lisa Wong, EM Program Director, comments: “The combination of VR simulation and traditional clinical teaching has transformed our residents’ preparation for critical cases. They’ve had the opportunity to manage each scenario multiple times before facing it in real life.”
Surgical Training
Surgical education has perhaps benefited most dramatically from modern approaches, particularly for complex procedures requiring fine motor skills and spatial awareness.
Case Study: University Surgical Program implemented a VR-enhanced training program for laparoscopic procedures:
- Residents achieved competency in 45% less time
- Complication rates during initial procedures decreased by 62%
- Operating time for new surgeons decreased by 28%
- Faculty reported spending 35% more time on advanced techniques rather than basics
First Responder Training
First responders face unique training challenges, often working with limited resources in unpredictable environments.
The Red Cross implemented a blended training program combining traditional hands-on practice with VR scenarios for mass casualty events. Results included:
- 73% improvement in triage accuracy
- 45% reduction in time to establish effective incident command
- 68% higher confidence ratings among participants
- 52% better retention of protocols at six-month follow-up
Implementation Strategies: Integrating the Best of Both Worlds
The most effective medical education programs integrate traditional and modern approaches. Based on successful implementations across multiple institutions, these strategies have proven most effective:
1. Spiraling Curriculum Design
Create a progressive curriculum that spirals between theoretical knowledge, simulation practice, and clinical application:
- Begin with foundational knowledge through interactive lectures
- Follow with simulation/VR practice of basic skills
- Apply skills in supervised clinical settings
- Return to simulation for advanced skills and rare scenarios
- Progress to more independent clinical practice
2. Deliberate Practice Framework
Implement structured deliberate practice protocols:
- Break complex procedures into component parts
- Provide precise metrics for each component
- Ensure multiple repetitions with feedback
- Gradually increase difficulty and complexity
- Integrate components into complete procedures
3. Faculty Development
Success requires faculty who understand both traditional and modern approaches:
- Train clinical faculty in simulation and VR facilitation
- Develop specific debriefing skills for simulation exercises
- Create faculty incentives for educational innovation
- Establish communities of practice for educator development
Conclusion: The Future of Medical Education
The future of medical education lies not in choosing between traditional and modern approaches, but in thoughtful integration that leverages the strengths of each. The evidence clearly demonstrates that combined approaches yield superior results in learning efficiency, knowledge retention, and clinical performance.
As we look ahead, several principles should guide medical education development:
- Patient-centered focus: Both traditional and modern approaches must ultimately serve the primary goal of improving patient care
- Evidence-based education: Apply the same rigorous standards to educational methods that we demand of clinical interventions
- Continuous innovation: Embrace new technologies while maintaining the human connection that remains essential to medicine
- Accessibility: Work to ensure modern educational approaches become more affordable and accessible to all healthcare professionals
The practitioners who will excel in tomorrow’s healthcare environment will be those who embrace both the wisdom of traditional medical education and the enhanced learning opportunities of modern approaches. By combining the best of both worlds, we can create a new generation of healthcare providers equipped to meet the challenges of 21st century medicine.